
Africa is home to 93% of the world’s malaria cases and 94% of the world’s malaria deaths (WHO, 2019). In 2018, there were 228 million cases and 405,000 deaths from malaria globally.
Pregnant women and children under the age of 5 are most at risk. A child still dies every two minutes from malaria.
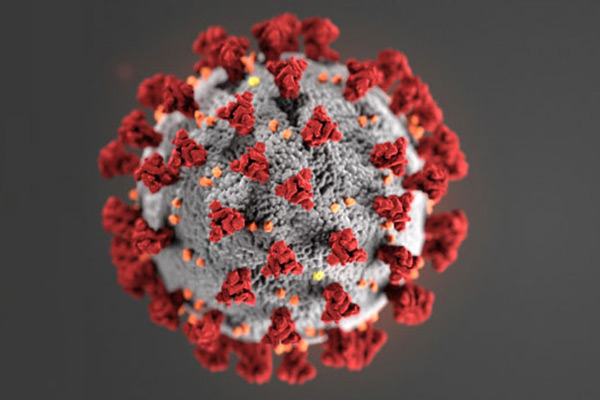
In the African region, which carries more than 90% of the global malaria burden, 45 countries out of 54 have reported cases of COVID-19 as of 23 April 2020.
For both malaria and COVID-19, this presents an overwhelming crisis politically, economically, financially, socially and culturally…..the norms we have structured our lives comfortably around and have adhered to have changed overnight.
Malaria can be prevented, diagnosed and treated. Similarly, COVID-19 can be prevented, diagnosed and treated. Africa must continue to place emphasis on malaria prevention, treatment and control in the era of COVID 19.
However, unlike COVID – 19, over the years we have developed, tried and tested diagnostic protocols to prevent, diagnose and treat malaria.
Important lessons have been learnt in terms of targeted advocacy, community engagement, surveillance methods and this knowledge should be shared in this COVID-19 era. This is a fight we can win if we work together.
As the world rightly focuses on the COVID-19 pandemic, it is important to ensure that efforts in combating malaria are not neglected.
The malaria community must remain committed to supporting the prevention of malaria infection, illness and death through preventive and case management services, whilst maintaining a safe environment for patients, clients and staff.
Deaths due to malaria and its comorbidities (anaemia, undernutrition, etc.) must continue to be addressed
There is a growing risk that malaria deaths will rise during the COVID-19 outbreak, if malaria control programs are postponed, and parents refrain from taking sick children to health clinics out of fear of COVID-19 infection.
The COVID-19 pandemic further challenges malaria responses and aggravates the plight of those most vulnerable to and affected by malaria.
Pregnant women, infants and children in malaria endemic areas are facing multi-fold increase in their vulnerability to malaria, whilst nationwide lockdowns and curfews are in place to control the spread of COVID19.
Continued investments to eliminate malaria will pay dividends beyond this one disease alone by alleviating a significant burden on resource-constrained health systems.
To achieve this, we need to increase domestic resources towards strengthening our health systems and malaria programs.
We must urgently shore up the world’s systems for health, particularly in the most vulnerable countries, to prevent COVID-19 from devastating communities and derailing lifesaving malaria programs.
Effective and efficient healthcare systems are critical for both – to end malaria as an epidemic and to fight COVID-19 as a pandemic.
This includes enhanced detection and case findings, access to treatment to interrupt malaria transmission and to reduce community transmissions for COVID-19.
Even as COVID-19 is disrupting our health systems, we must ensure continuity of service delivery for malaria. Supply chains for treatments and other tools to fight malaria must be maintained and protected and we need to begin planning now for contactless systems for accessing treatments and care to protect patients and the healthcare workers whose efforts are already stretched and will be more so in the coming months.
After years of progress, the number of malaria cases is on the rise – and the COVID-19 pandemic threatens to further derail hard-won gains.
As health advocates, let us amplify our voices as we speak up for enhanced malaria responses at the same time as we advocate for better detection and treatment of COVID-19.
Authors: Dr Sylvia Anie, CSci, FRSM, FRSC (Advisor, Youth Leaders for Health)
Augustine Kumah, MPH (Youth Leader for Health, Ghana)


















Facebook
Twitter
Pinterest
Instagram
Google+
YouTube
LinkedIn
RSS